The Unintended Consequences of Handwashing in Healthcare Sinks Can Contribute to HAIs
Sinks can contribute to HAIs
Sometimes we think that we know all there is to know. But real growth comes from realizing that you only know what you know, regardless of your experience. Are you in the trap of thinking you know all there is to know about the sinks in every patient’s room, in every treatment area and every critical care area of the hospital?
For instance, all you know about a hospital sink is what you can observe in 10 seconds. Is it clean or dirty? Does the tap work with running hot and cold water? Is the drain free running or slow?
The literature is replete with articles and studies in infection prevention annals extolling the virtues of various environmental hygiene products, processes, and programs. There are far fewer articles and studies in those same annals discussing sinks as a source of potentially deadly organisms. However, are you aware of the published articles and studies implicating sinks in the spread of dangerous bacteria that could lead to Hospital-associated Infections (HAIs)?
IN THE NEWS
New infection prevention guidelines, recently issued by several organizations, tackle fingernails, sinks, and cracked hands.
Among the recommendations, published in Infection Control & Hospital Epidemiology, from the Society for Healthcare Epidemiology, the Infectious Diseases Society of America, the Association for Professionals in Infection Control and Epidemiology, the American Hospital Association, and the Joint Commission are:
Healthcare workers should cut their fingernails so they don't extend beyond the fingertips, and should keep them natural.
Patient-facing healthcare workers should avoid washing their hands so much that they become dry and cracked, which can lead to cuts or bruising and infection, putting the patient and the provider at risk. Instead, alcohol-based hand sanitizers should be used.
Hospitals should install hand sanitizer dispensers not just on the inside or outside of each patient room, but in both places.
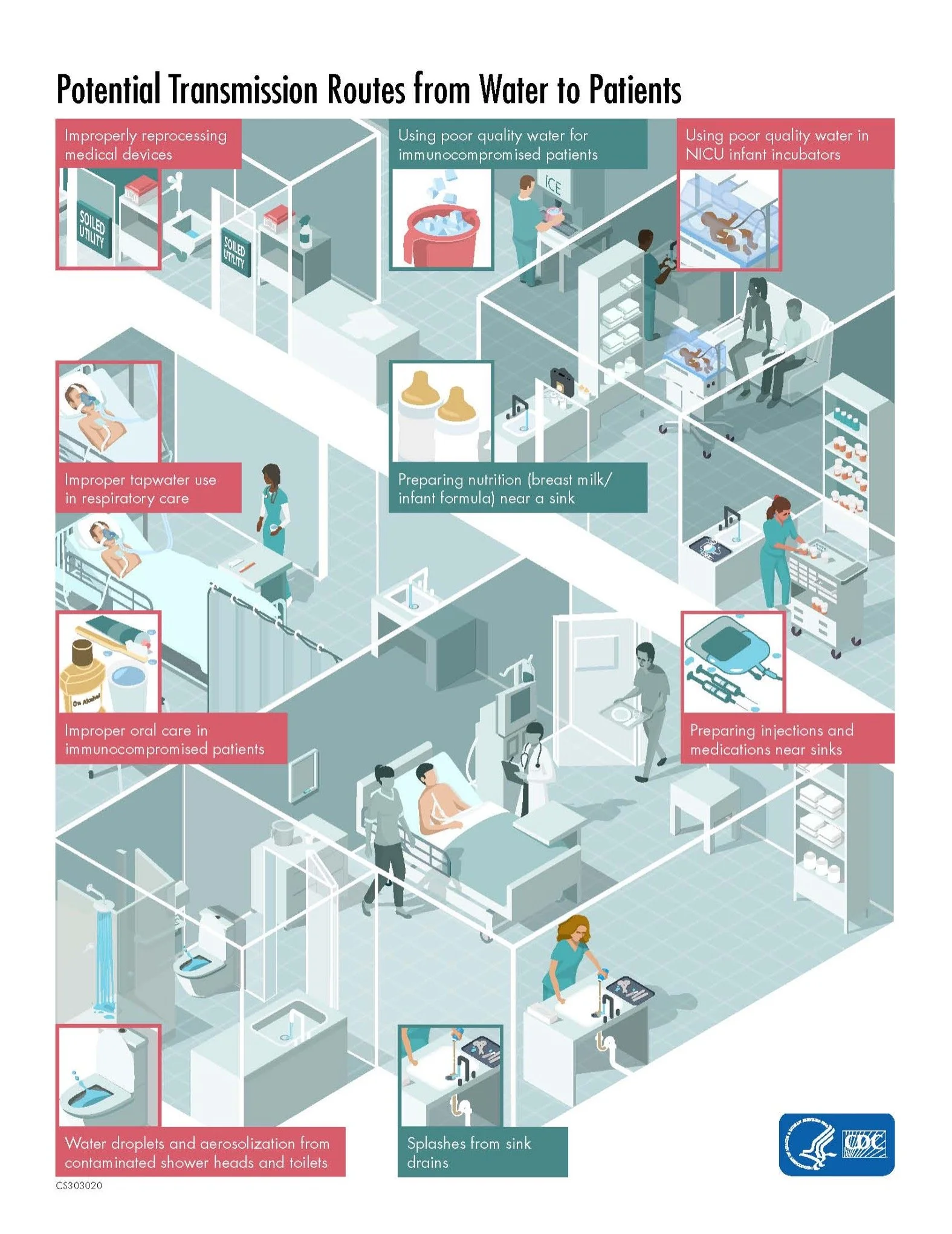
Certain basins should be dedicated to hand-washing alone, with no other fluids being dumped into them, to avoid infectious organisms splashing onto the counter or becoming aerosolized. Instead, use a toilet or a dedicated receptacle for other fluid disposal purposes.
Instead of cleaning sink drains with a splash of bleach -- now common practice -- use products newly approved by the U.S. Environmental Protection Agency specifically capable of removing biofilm.
The advisories are based on new evidence showing previously unappreciated ways that various pathogens can spread in healthcare settings. They are most appropriate for hospitals, but are applicable to long-term and ambulatory care settings, including dialysis facilities, said lead author Janet B. Glowicz, PhD, RN, of the CDC, in an interview with MedPage Today during which a CDC public relations representative was present.
The CDC participated in the guidelines' development, the latest in a 40-year series since 2014.
One of the most important recommendations has to do with new recognition of how pathogens can spread through "premise plumbing" i.e., the hospital's sinks.
One of the most important recommendations has to do with new recognition of how pathogens can spread through "premise plumbing ," i.e., the hospital's sinks.
"Nurses in particular don't realize that all the stuff they're putting down those sinks can create biofilms and can also create resistant bacteria, and that can be aerosolized and contaminate the patient environment," Glowicz said.
IS THERE MORE YOU CAN LEARN ABOUT THE PROBABLE LINK BETWEEN SINK DRAINS AND HAIs?
Proper hand hygiene is one of the pillars of infection prevention and control in hospitals. Patients receiving healthcare have faced the ongoing threat of infections and antibiotic-resistant organisms potentially spread by contact with the hands of Healthcare Personnel (HCP).
Interaction with the healthcare environment can result in hand contamination following activities as brief as touching a bed rail. Hospitals have experienced increases in numbers of patients colonized with extended-spectrum β-lactamase–producing Enterobacterales were noted, while the incidence of carbapenem-resistant Enterobacterales remained stable.
While Covid was the most concerning infectious disease for two years, healthcare facilities have experienced the emergence of Candida auris, a resistant fungus that is wreaking havoc on hand touch surfaces.
In a devilish case of unintended consequences, sinks have been linked to a number of outbreaks of serious infections in hospitals from Baltimore to Shanghai and many places in between in recent years. In one notable case, a hospital in the Netherlands took sinks out of the patient rooms in its intensive care unit in a bid to slow the spread of bacteria. (It worked.)
A patient’s #1 Fear of being admitted to a hospital is GERMS. Hospital-associated infections are a serious problem, and you might not know the real toll of lives affected by Multiple Drug-Resistant Organisms (MDROs).
UNDER-REPORTED DEATH TOLL DUE TO HOSPITAL-ASSOCIATED INFECTIONS
Even when recorded, tens of thousands of deaths from drug-resistant infections – as well as many more infections that sicken but don’t kill people – go uncounted because federal and state agencies are doing a poor job of tracking them. The Centers for Disease Control and Prevention (CDC), the go-to national public health monitor, and state health departments lack the political, legal, and financial wherewithal to impose rigorous surveillance.
Here are the facts regarding hospital-associated infections (HAIs) in America. In 2019 (the most recent year with data), there were 36,242,000 admissions to U.S. hospitals. A conservative standard HAI rate in a hospital is 7% (of admitted patients will get an HAI during their stay). But there are hospitals with an HAI rate of 10% or more.
Doing the math, 7% of 36.2 million admissions=2.5 million patients get an HAI while 10% of 36.2 million admissions=3.6 million patients get an HAI while hospitalized.
If the mortality rate for 2.5 million patients is 10%, 250,000 Americans die of HAIs. If the same mortality rate of 10% is applied to 3.6 million HAIs, the number of patient deaths us 360,000. This would place deaths due to HAIs as the #3 on the causes of death in the U.S. just behind heart disease and cancer.
This estimated deaths due to HAIs is considerably higher than the 99,000 that the Centers for Disease Prevention and Control (CDC) reports on their website and is cited by many reputable papers.
Drug-resistant infections are left off death certificates for several reasons. Doctors and other clinicians get little training in how to fill out the forms. Some don’t want to wait the several days it can take for laboratory confirmation of an infection. And an infection’s role in a patient’s death may be obscured by other serious medical conditions.
There’s also a powerful incentive not to mention a hospital-associated infection: Counting deaths is tantamount to documenting your own failures. By acknowledging such infections, hospitals and medical professionals risk potentially costly legal liability, loss of insurance reimbursements and public-relations damage.